Approximately 1% of people worldwide suffer from the autoimmune condition celiac disease. Grain allergies and loss of nutrients occur when a person with celiac disease consumes gluten, a protein present in grains such as wheat, barley, and rye that damages the small intestine. However, the symptoms of celiac disease can vary greatly, making a diagnosis difficult without testing. This comprehensive guide will cover every aspect of celiac disease, including symptoms and signs, who are most at risk, appropriate tests for diagnosis, and management strategies for this progressive illness.
What Exactly is Celiac Disease?
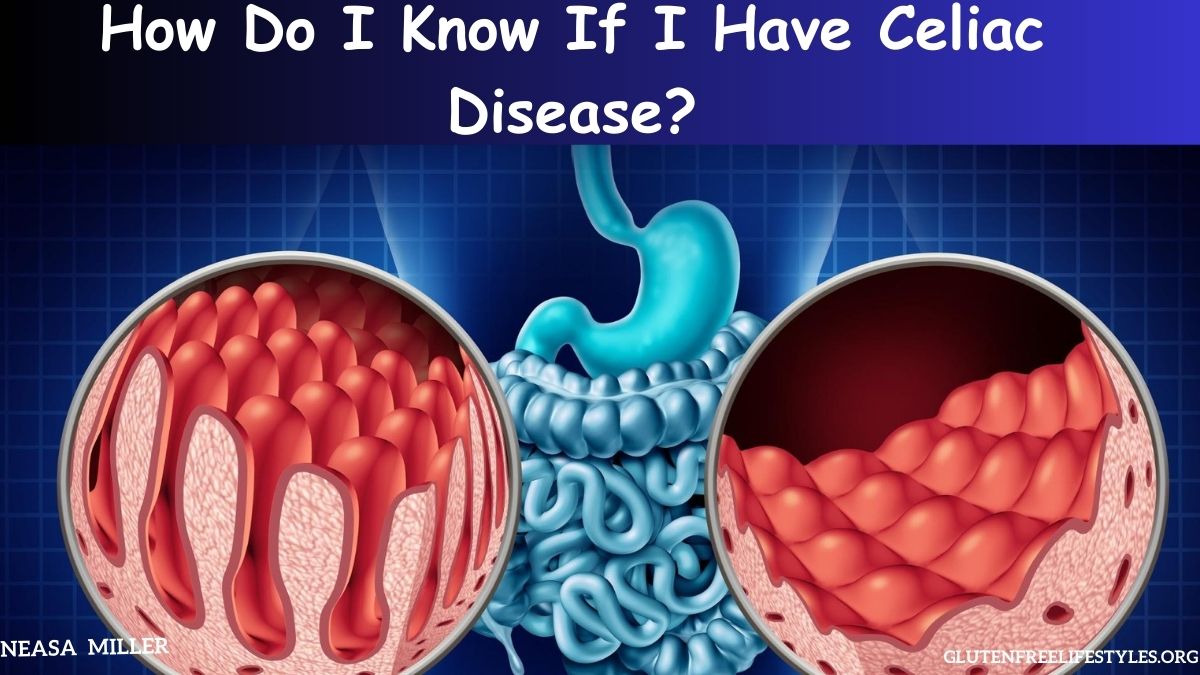
A dangerous inherited autoimmune condition called celiac disease causes damage to the small intestine when gluten is consumed. This illness prevents the body from absorbing nutrients by gradually killing the villi, the finger-like projections that line the small intestine and take up nutrients from meals. Gluten causes an immunological response in celiac disease sufferers that damages the villi in the intestines.
Protein, fat, carbs, vitamins, and minerals are essential macro- and micronutrients lost from meals when the villi deteriorate. Over time, the body develops symptoms from the malabsorption of these vital vitamins and minerals, which also worsens nutritional deficits. Although celiac disease was formerly thought to be extremely rare, it currently affects around 1 in 100 individuals worldwide, although it is still incredibly underdiagnosed.
What Are the Symptoms of Celiac Disease?
Celiac disease impacts every system of the body, consequently, symptoms are highly variable and differ greatly among patients. Some of the common symptoms include:
Gastrointestinal Symptoms:
- Chronic diarrhea, constipation, bloating or abdominal pain
- Floating stools due to fat malabsorption
- Gas, cramping, or distention after meals
- Unexplained weight loss or weight gain
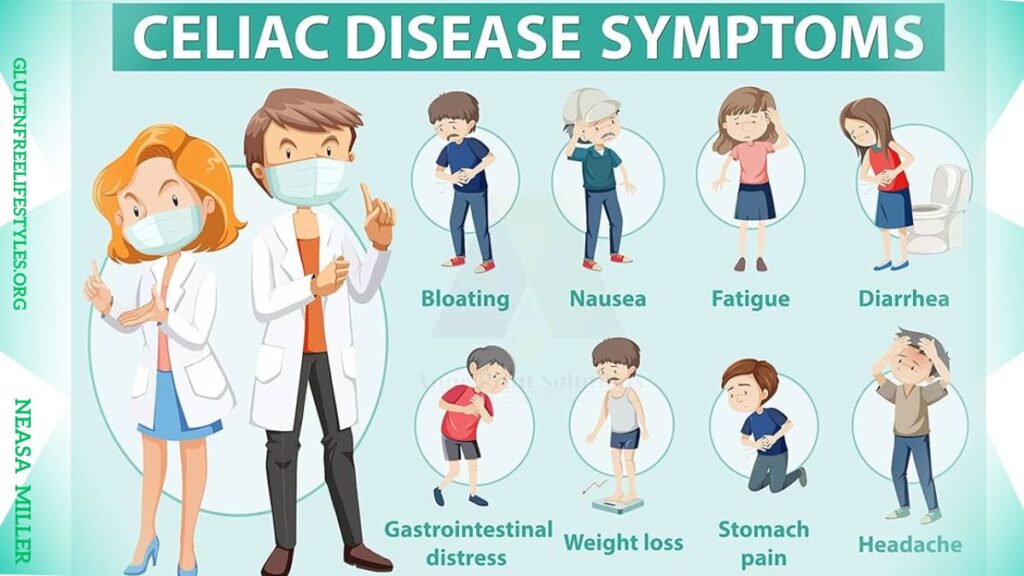
Nutritional Deficiency Symptoms:
- Anemia (iron deficient)
- Weakness, fatigue, and headaches
- Bone pain or bone loss (osteoporosis)
- Joint pain, muscle cramps, and leg swelling
- Bleeding issues, and bruising easily
- Mouth ulcers or canker sores
- Tingling or numbness
Skin Conditions:
- An itchy skin rash called dermatitis herpetiformis
- Aphthous ulcers (canker sores)
Children with celiac often show alternative symptoms like:
- Failure to thrive through lack of nutrient absorption
- Delayed puberty, lack of growth, or short stature
- Dental enamel defects and discolored teeth
Other Issues:
- Neurological problems like depression and anxiety, migraines, epilepsy
- Infertility, pregnancy complications, or repeated miscarriage
- Liver conditions like abnormal liver enzymes or fatty liver
Autoimmune Disorder Overlap:
Due to its genetic autoimmune nature, celiac disease is associated with several other autoimmune conditions including:
- Type 1 diabetes
- Thyroid diseases such as Grave’s or Hashimoto’s
- Rheumatoid arthritis
- Addison’s disease
- Sjogren’s syndrome
If you have symptoms of related autoimmune conditions in addition to issues like malnutrition, anemia, or intestinal distress this greatly increases suspicion for celiac. Talk to your doctor about associated conditions.
Who is Most at Risk for Celiac Disease?
Celiac has a strong hereditary component, meaning first-degree relatives (parents, children, siblings) of those with celiac are at the highest risk. However, only 30-50% of genetic relatives develop celiac. Beyond family history, additional genetic, medical, and environmental factors that increase risk include:
Genetic Risk Factors:
- HLA-DQ2 gene variant: Present in 95% of celiac cases
- HLA-DQ8 gene variant: Most of the remaining celiac cases
- First-degree family members
Medical Conditions Associated with Increased Risk Include:
- Type 1 diabetes or autoimmune thyroid
- Down or Turner genetic syndromes
- Microscopic colitis or pancreatic insufficiency
- Rheumatoid arthritis, lupus, or Sjogren’s
- Addison’s disease or alopecia areata
Environmental Triggers:
- Infections such as rotavirus increase the likelihood
- Intestinal surgery, pregnancy, emotional trauma
- Early or high-quantity introduction to gluten
Keep in mind, that while these factors increase risk, they do not guarantee someone will develop celiac disease. Many have the HLA genes or thyroid disease and tolerate gluten just fine. But for those with ongoing health issues, these clues may justify celiac screening.
Diagnostic Testing for Confirming Celiac Disease
Due to the wide range of symptoms that can mimic scores of other conditions, getting properly diagnosed with celiac is complex and often delayed by years. However, with greater awareness and improved screenings, more mild or non-classical cases are diagnosed sooner. Confirmation requires 3 components: Blood tests, genetic testing, and intestinal biopsy.
Blood Tests:
Serological blood tests check for antibodies associated with the abnormal gluten immune reaction in celiac disease. The primary antibodies include:
- IGA (anti-tissue Transglutaminase) – The preferred single test, checks for IgA antibodies to tissue transglutaminase enzyme. High sensitivity.
- EMA (anti-endomysial) – Checks for IgA antibodies towards smooth muscle endomysium tissue. Particularly for celiac diagnosis but has lower sensitivity.
- DGP (anti-deamidated gliadin peptides) – Measures IgA & IgG antibodies response to gliadin portion of gluten protein.
- Total serum IgA level: This must be measured as well because 3% of celiacs are IgA deficient and tests can miss them. For IgA deficient patients, IgG based testing is crucial.
Most physicians will start with the tTGA screen, and if abnormally high they will order confirmatory EMA or DGP along with total IgA tests. Keep in mind, that no blood test is perfect, false negatives are possible if gluten intake was too low preceding the test. Periodic retesting may be warranted with extreme suspicion.
Genetic Testing:
Though not required for diagnosis, genetic testing helps evaluate the risk and likelihood of celiac development. Tests identify HLA genes HLA-DQ2 and HLA-DQ8, present in almost all celiac cases. While largely used for excluding celiac diagnosis in antibody-negative patients, gene variants can support diagnosis when borderline or inconclusive antibody results occur. Genetic risk alone does NOT mean someone will develop celiac disease – over 30% of the population carries HLA genes but less than 1% develops celiac disease. Genetic results should be evaluated regarding symptoms and celiac antibody blood testing.
Intestinal Biopsy:
Even with positive antibody tests, a small intestinal biopsy is required to confirm damage and flattening of intestinal villi consistent with celiac disease. Multiple samples from duodenum tissue will be evaluated to stage the degree of villous atrophy. Any degree of villous blunting (Marsh stage 1-3) in conjunction with positive celiac antibodies confirms disease diagnosis.
Can Celiac Disease Develop Later in Life?
Celiac disease is a condition that can readily strike later in life. Furthermore, you might be surprised to learn that as you age, your risk of developing celiac disease rises dramatically. Numerous recent research has also discovered a clear correlation between the intensity and age of celiac disease symptoms.
There is a correlation between increasing age and celiac disease that can be attributed to four main factors: prior surgery, antibiotic use, increased infection rate, and stress. The microbiome and bacterial makeup of our guts alter as we age. Celiac disease may potentially result from this event.
How to Manage Celiac Disease
Since celiac disease is a systemic autoimmune illness caused by dietary gluten proteins, the only recognized medical treatment is a rigorous lifelong gluten-free diet that reduces the possibility of developing new autoimmunities while also relieving symptoms and healing intestinal damage. Intestinal villi can heal fully or partially when gluten sources like wheat, barley, rye, and occasionally oats are eliminated from the diet. This necessitates being meticulous when reading ingredient labels, being aware of any hidden gluten sources, and avoiding cross-contamination both at home and when eating out.
For individuals who have just received a diagnosis, consulting with a qualified nutritionist or dietitian who has had specialized training in celiac disease can be extremely helpful in navigating a gluten free lifestyle and avoiding drastic lifestyle adjustments. Most patients report considerable symptom relief and restored vitality and energy within weeks to months of strict gluten avoidance. Long-term management of celiac disease requires strict diet adherence, routine blood work, and attentive medical attention.
The Takeaway
If you or a loved one experiences chronic gastrointestinal distress, constant fatigue, unexplained anemia or nutrient deficiencies, failure to thrive, enamel defects in children, or associated autoimmune conditions, ask your doctor about screening for celiac disease, especially if you have a family history. Left untreated, celiac disease can result in serious gastrointestinal cancer, osteoporosis, infertility, neurological conditions and other autoimmune disorders. Diagnosis and gluten free management significantly minimize these threats while providing symptom relief and improved well being. Partner closely with your medical team if celiac is suspected – early recognition and treatment provide the best opportunity for health.
Related Posts

I’m Neasa Miller, a professional dietitian with 5 years of experience. I founded glutenfreelifestyles.org to assist people online in embracing gluten-free living. Read more about me